What is cervical cancer?

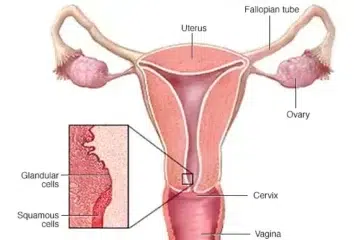
Cervical cancer kicks in when abnormal cells start their unwelcome party in the lining of the cervix. The headliner here is squamous cell carcinoma, which hogs the spotlight with about 70% of cases. Then there’s adenocarcinoma, a bit more elusive and rare, clocking in at around 25%. It’s a sneaky one because it sets up shop higher in the cervix, making it harder to catch.
Fast forward to 2023, and over 900 folks got hit with a cervical cancer diagnosis, usually around their 50th birthday.
But hey, there’s some good news!
Thanks to the National Cervical Screening Program that kicked off back in ’91 and the national HPV vaccine program launched in ’07, we’ve seen a drop in cervical cancer cases.
High fives all around for modern medicine!
Curious about how Cancer Council researchers are hustling to help Australia kick cervical cancer to the curb? Keep reading.
Types of Cervical Cancer
So let’s break down these two main troublemakers: squamous cell carcinomas and adenocarcinomas.
Squamous cell carcinoma is like that overly popular kid at school—making up about 80% to 90% of all cases. Adenocarcinomas? They’re more like the quiet ones hanging out on the sidelines—only accounting for about 10% to 20%.
How common is cervical cancer?
Every year in the U.S., around 14,000 new cases of cervical cancer pop up. It tends to rear its ugly head most often in folks between 35 and 44 years old, with the average age at diagnosis being about 50. Sadly, it’s estimated that nearly 4,000 people lose their lives to this disease annually. What’s even more troubling is that despite advancements in HPV screenings and vaccinations, these numbers are still climbing. It’s a sobering reminder of how crucial early detection and prevention really are.
signs and symptoms
Early changes in cervical cells typically do not present any symptoms. The most effective way to detect abnormal cells that could potentially develop into cancer is through a cervical screening test. If these early changes progress to cancer, you might notice the following symptoms:
- Bleeding between periods
- Periods becoming longer or heavier
- Pain during sex
- Bleeding after sex
- Pelvic pain
- Changes in vaginal discharge, like more or odd color/smell
- Bleeding after menopause
These signs might be from other issues, but if you’re worried or symptoms stick around, talk to your doctor. This is important for everyone with a cervix, no matter your sexual orientation or gender identity.
What causes cervical cancer?
Most cervical cancers are caused by HPV, the Human Papillomavirus, which is a sexually transmitted infection. HPV is transmitted by anal, oral, or cervical sexual activities and the risk of developing cancer is high. Many of our patients get HPV at some point, and in the majority of cases, their body takes up the fight to get rid of the infection without them knowing. Cervical cells switching to cancer, however, is a clear sign that the body cannot fight it.
There are over 100 types of HPV, with a dozen or so responsible for causing cervical cancer. Identifying these specific HPV types early is crucial for preventing the development of cancer.Regular checkups with your healthcare provider can often detect cell changes at an early stage before they become cancerous. Getting the HPV vaccine would be another way to prevent infections of this virus and of the specific types accountable for 90% of all cervical cancer cases.
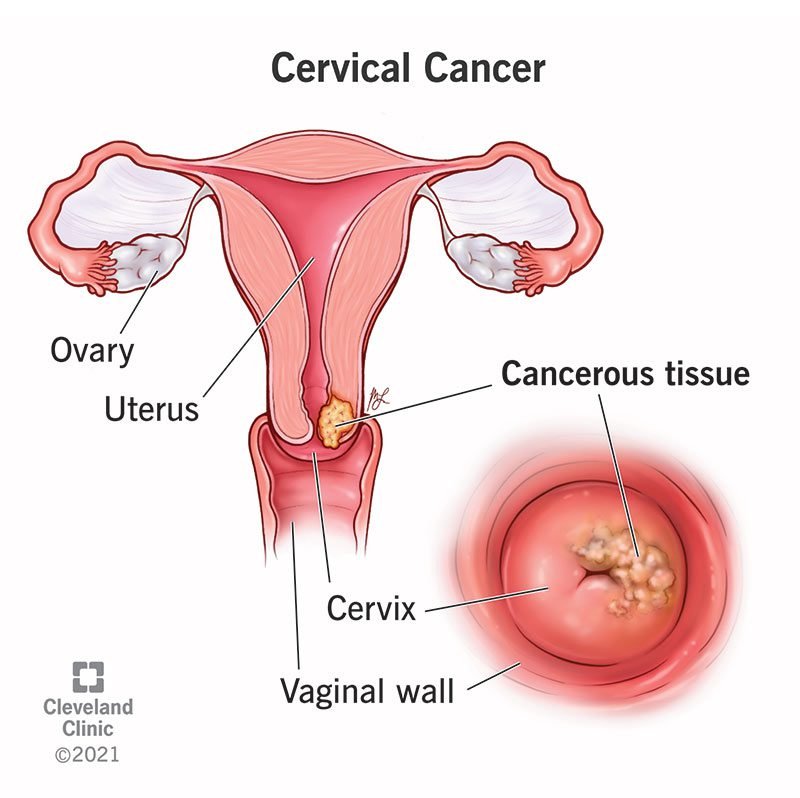
Diagnosis
In case, the screening test hints at the potential of developing a cancer tumor in you then you will be referred to this specialist.
The main tests for diagnosing cervical cancer are: The major tests that can be used to diagnose cervical cancer are the two, namely: the Pap smear test as well as the colposcopy.
Colposcopy with Biopsy:
A colposcopy is a procedure that shows which cervical cells are asize.
Vagina is sampled through introduction of a speculum, and using a device which resembles a telescope, known as a colposcope, the doctor gains a vantage point over the things found in the vagina.
In case something seems more suspicious, the colposcopist may be a gynecologist or a nurse practitioner who will then take a piece of tissue from the area using a biopsy instrument to check under the lens.
Large Loop Excision of the Transformation Zone (LLETZ) or Cone Biopsy: LLETZ stands for ‘Large Loop Excision of the Transformation Zone’ and the Cone Biopsy is another procedure which is slightly different as it involves the removal of a cone-shaped piece of cervical tissue, usually used when the growth is larger or when the cervical canal is involved.
In the event you experience a precancerous change then you may undergo either a LLETZ or a cone biopsy.
LLETZ also eradicates the cervical tissues that are used for sampling and therapy and LLETZ women are often anesthetized locally.
Cone biopsy is for the glandular tissue in the cervix that has increased cellularity with atypical appearance or has features suggestive of early carcinoma.
Another of the processes that implies a great number of tests in order to reveal the issue.
Treatment
When cervical cancer is diagnosed, we regarding the cervical cancer into stages one to four. Stage 1 means that cancer is only found in the cervix and has not spread to the pelvic region. The stage 4 suggests that the cancer is in its advanced form and it has affected areas of the lung, liver, and/or bones. In this way, in the process of aseptic ization, physicians will, without fail, have chosen an optimal treatment for you.
The treatment plan varies based on the stage of the disease:The treatment is differentiated according to the tumor progression because the stages of cancer differ dramatically in their outcomes.
- Early and Small Disease (less than 4cm): Promoting more involvement of different types of public transport and electric vehicles among our residents will also play a massive role in cutting down the carbon pollution from the transport segment.
Treatment: Chemoradiation therapy follows surgery in most cases, with surgery being the mainstay.
Details: For a few small-sized tumors, a cone biopsy may be adequate but a few may require a hysterectomy, the surgical removal of the uterus.
2. Locally Advanced Disease:
Treatment: RADIO THERAPY/RADIATION THERAPY often complementary with chemotherapy / cisplatin (cisplatin).
3. Metastatic Disease:
Treatment: , platinum/fluorouracil the most frequently used or when no other treatment is applicable – the only available treatment modality for some patients.
The consideration of stage ensures that the treatment offered is accorded and given in a manner that is befitting the ailment hence the perfect care for any disease.
Preventing cervical cancer
HPV Vaccine
The HPV vaccine is effective protection against HPV, which is responsible for most cervical cancer strains. Gardasil 9 is developed to prevent cervical cancers by targeting nine HPV types that account for 90% of cervical cancer cases. Most girls and boys in Australia whilst in school are vaccinated through the National Immunisation program where the HPV vaccine is usually administered to 12-13 years and under. It is available to any individual aged between 12-25 years and is taken once as a shot injection.
Regarding the use of the HPV, one may find more information [here](link to more information).
HPV vaccination does not replace Cervical Cancer Screening Test, so you should continue having it. If one has been immunized against HPV, he or she should go for a first screening at age 25 and then repeat this after every five years only. For more precise information on cervical screening, visit Cancer Council.