“Fatty Liver Facts: What You Need to Know is one of the articles featured in the lesson plan on the Common Core State Standards, whose topic is presented in the following way:
Doctors decided to give Non-Alcoholic Fatty Liver Disease (NAFLD) a new Clinical term in 2023 known as Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) Its new name is NAFLD when there is the buildup of fat in the liver and at least one factor for metabolism disease. Moderate drinking refers to the use of alcohol in moderate proportions and is called MetALD. For reasons of clarity, MetALD should be distinguished from Alcoholic Liver Disease or more simply, Disease due to pure alcohol alone.
Formerly, they used to term it as Non-Alcoholic Fatty Liver (NAFL) and Non-Alcoholic Steatohepatitis (NASH, now MASH) to make people realize that this disease is very dangerous. They used to refer to the situation when there was more inflammation in the liver as NASH, but now they speak of MASH. NAFL is the slightly simplified term, and normally it is not progressive. However, in the long run, in case of worsening of a condition, the following complications may develop: cirrhosis, liver cancer, liver failure, and potentially heart diseases.
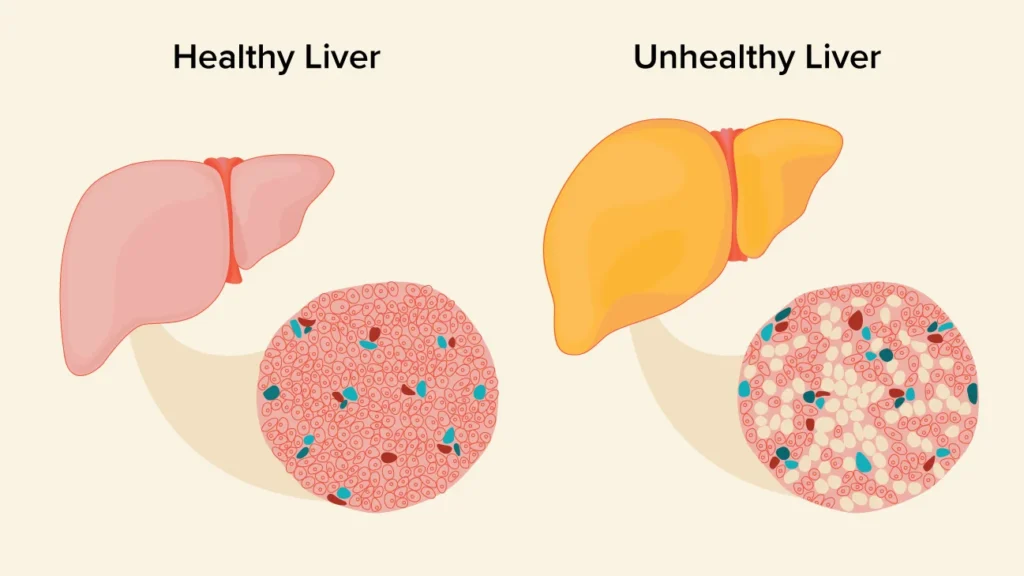
Others include being very overweighed and suffering from type 2 diabetes since they predispose the individual to MASLD. Other risks are obesity, having a condition called metabolic syndrome which means having at least three of the five heart disease precursors including a large waist size, high blood pressure, high blood sugar, high triglycerides, and low HDL cholesterol, consuming large amounts of fructose and advancing age. MASLD may be diagnosed by comparing a sample of the liver to a healthy liver but doctors might need to ensure there are no other causes for a fatty liver before doing this.
Nonalcoholic Fatty Liver Disease:
Types of fatty liver disease
Healthcare professionals categorize fatty liver disease into two types. When there’s only fat accumulation without liver damage, it’s referred to as nonalcoholic fatty liver disease (NAFLD). or if you have signs of inflammation and liver cell damage, the disease is called nonalcoholic steatohepatitis (NASH).
10% to 20% of Americans have NAFLD. About 2% to 5% have NASH
Symptoms
Fatty liver disease is occasionally referred to as a silent liver condition. That’s because it can happen without showing any signs. Most folks with NAFLD have fat in their liver, but it doesn’t harm the liver. A few people with a fatty liver might end up with NASH.
In individuals with NASH, symptoms may take years to manifest. If NASH damages your liver and makes it scarred and hard, that’s called cirrhosis.
- Feeling extremely tired
- Weakness
- Losing weight
- Skin and eyes turning yellow
- Spider-like blood vessels on the skin
- Itchy skin that lasts a long time
When NASH turns into cirrhosis, it can bring more symptoms like holding onto extra fluids, internal bleeding, losing muscle, and feeling confused. Over time, people with cirrhosis might face liver failure and might need a new liver through a transplant.
Who’s at risk
Genetics
In families where diabetes type 2 runs in the genes, about two-thirds of them have more than one family member dealing with MASLD. If someone in the family has MASH, there’s a higher chance that others might face fibrosis. Asians are more likely to have metabolic syndrome and MASLD compared to people in the West. Among different ethnic groups, Hispanic individuals are more likely to have MASLD than white individuals, while black individuals have the lowest chances.
Certain gene differences, specifically in PNPLA3 and TM6SF2, are linked to MASLD. These genes are connected to both the presence and seriousness of MASLD, but it’s not entirely clear how they can help in diagnosing the condition. Even though there’s a genetic side to NAFLD, the American Association for the Study of Liver Diseases (AASLD) doesn’t recommend routinely testing family members because there’s still uncertainty about how much it’s inherited, despite some evidence from family and twin studies.
From diet
As per experts in the Asia-Pacific region, excessive food intake plays a significant role in MASLD and MASH, particularly among individuals who are not overweight. The kind and amount of food you eat, like omega-6 fatty acids and fructose, play a big role in how MASLD can turn into MASH and fibrosis. Also, not getting enough choline in your diet can lead to MASLD.
Eating a lot of processed, red, and organ meats is linked to a higher chance of getting MASLD. Some studies even suggest that eggs might be connected to MASLD. On the flip side, research shows that eating healthy plant foods like legumes and nuts is linked to a lower risk of getting MASLD. Two different studies found that eating a diet with lots of healthy plant foods and less animal foods is connected to a lower risk of getting MASLD, even when adjusting for BMI (body weight).
From lifestyle
Maybe, it is worthy to note that snoring everyday can be potentially dangerous to the development of MAFLD. If the snoring is loud than one could be suffering from a severe breathing disorder called Obstructive Sleep Apnea (OSAS). Lung diseases can cause the airways within the lungs to become blocked or narrowed – even for a few hours — and the blood may not contain enough oxygen. It can cause different changes in the body, including the inflammation of the tissues, insulin resistance, and liver damage due to the lack of this gas. Such a study based on a group of people during the time course of their life unveiled that those who snored frequently at any given age and were not obese had the highest risk of developing MASLD.
Diagnosis
Another thing that must be understood about the fatty liver disease is that it can develop in the background without becoming symptomatic. Generally, it is discovered by physicians during routine blood tests conducted on how the liver is functioning. especially if a woman with your size comes in with your test results and the doctor feels that something is off, fatty liver disease is likely to be a diagnosis that he or she will give you.
Specific tests like ultrasound or imaging scans can detect the presence of fat in your liver. This is why, some of the scans such as special ultra sound and MRI can ease identify if there is any scar tissue in the liver. However, the findings may suggest that there are other causes of liver ailments, and to rule out fatty liver as the sole cause, a liver biopsy is called for. During this, a needle is used to take a biopsy of the liver tissue and looked at under a microscope.
If fatty liver is combined with inflammation or damage, it is referred to as NASH, on the other hand if there is fat without inflammation or damage, then it is called NAFLD.
If there are nutrients and chemicals, fatty liver deposits, and inflammation, then it turns into NASH.
For instance, if, in the course of the disease, the liver has developed a specific type of fibrosis, this is an indication that the person is on the path towards cirrhosis.
Management
Treating NAFLD is essential, regardless of whether someone is overweight or not. MAFLD can be avoided, and there are guidelines from health organizations like the American Association for the Study of Liver Diseases (AASLD), American Association of Clinical Endocrinologists (AACE), National Institute for Health and Care Excellence (NICE), the European Association for the Study of the Liver (EASL), and the Asia-Pacific Working Party on NAFLD to help out.
Treatment
Treatment
If you have NAFLD without other health issues, you might not need special treatment. But making some changes to your lifestyle can help control or even reverse the fat buildup in your liver. These changes may include:
- Lose weight
- Bringing down your cholesterol and triglycerides
- Managing your diabetes
- Avoiding alcohol
Individuals with NASH do not have a specific medication to reverse the accumulation of fat in the liver. Occasionally, the liver may, damage stops or even goes backward on its own. But in other cases, the disease keeps moving forward. If you have NASH, it’s important to handle any conditions that could add to fatty liver disease.
- Lose weight
- Taking medicine to lower cholesterol or triglycerides
- Taking medicine to control blood pressure
- Taking medicine to manage diabetes
- Being careful with over-the-counter drugs
- Staying away from alcohol
- Consulting with a liver specialist
Some medicines that may help in managing Nonalcoholic steatohepatitis are being researched by scientists; example is antioxidants like vitamin E. They also ponders current uncontrolled diabetes medications for NASH, even though you are certainly not diabetic. However, only self-treat if you consult a liver specialist first and reconsider these medicines.
The main indirect concomitant of fatty liver disease is NASH to cirrhosis transformation. Cirrhosis is an irreversible process in which scarring and nodularity of liver tissue takes place.
When a condition warrants medical attention
If you conduct any form of fatty liver disease, ensure that this ranges your health care provider if have any signs suggesting the disease is escalating. Some of these symptoms include fatigue, loss of appetite but the generalized symptoms include weight loss, weakness, fluid retention or likely to bleed.
If there is ever an opportunity to be diagnosed with fatty liver disease, one must take time and effort to learn about one’s condition and communicate well with doctors. As most drugs can damage your liver in one way or another, accompany any illness with a doctor and disclose all your medication.

